
Anaesthesia, Climate and Sustainability
GOING GREEN

The specialty of anaesthesia is a significant contributor of three main greenhouse gases; carbon dioxide, nitrous oxide and fluorinated gases. In addition, the healthcare sector is a major producer of plastic waste. Travel, in the form of patient hospital visits, commuting hospital staff and the transportation of supplies, also contributes to a large carbon footprint. Even though the use of certain anaesthetic gases and plastic might be deemed necessary, is there anything the specialty, and patients, can do to reduce the impact on the environment?
This exhibition will explore these questions.
The medical journal, The Lancet, concluded in 2015 that the response to climate change could be “the greatest global health opportunity of the 21st century.” Despite this, Lancet Countdown, an expert group which monitors the links between climate change and health, reported in 2019 that although people are very interested in human health, it is rarely linked to climate change. The health profession must communicate the health risks of climate change and implement changes which will improve human health and wellbeing.
The climate crisis is a health crisis. A simple activity like going for a walk or enjoying the sunshine can expose people to harmful levels of pollution. Air pollution and high pollution days are linked to heart disease, stroke, asthma and lung cancer, contributing to around 500,000 premature deaths annually across Europe. Air pollution from roads in London alone costs £10.32 billion every year in terms of illness and pollution-related deaths. Just think what could be done with that money if air pollution was drastically reduced.
Rising temperatures and extreme weather events, such as flooding, increase the chance of infectious diseases spreading. Hot weather itself causes deaths. Diseases carried by ticks, such as Lyme disease, are expected to become more common in the UK with a rise in temperature, as well as other diseases, such as those carried by mosquitoes.
These factors all place pressure on the health profession. In 2020, the NHS launched their ‘Greener NHS’ campaign to tackle the health emergency. The NHS long term strategy sets out their commitment to making improvements to procedures, pharmaceuticals, carbon footprint, energy use and waste. As patients, we have a role to play too.
NHS impact on the environment
Climate change (or global warming) is the process of the earth heating up. When you receive an anaesthetic, many of the gases used to anaesthetise you are contributing to greenhouse gas emissions, and drugs such as antibiotics are being found in waterways. As patients receiving elective or emergency surgery, journeys for pre- and postoperative appointments and hospital admissions leave a carbon footprint, a footprint which is increased by the health professionals looking after you.
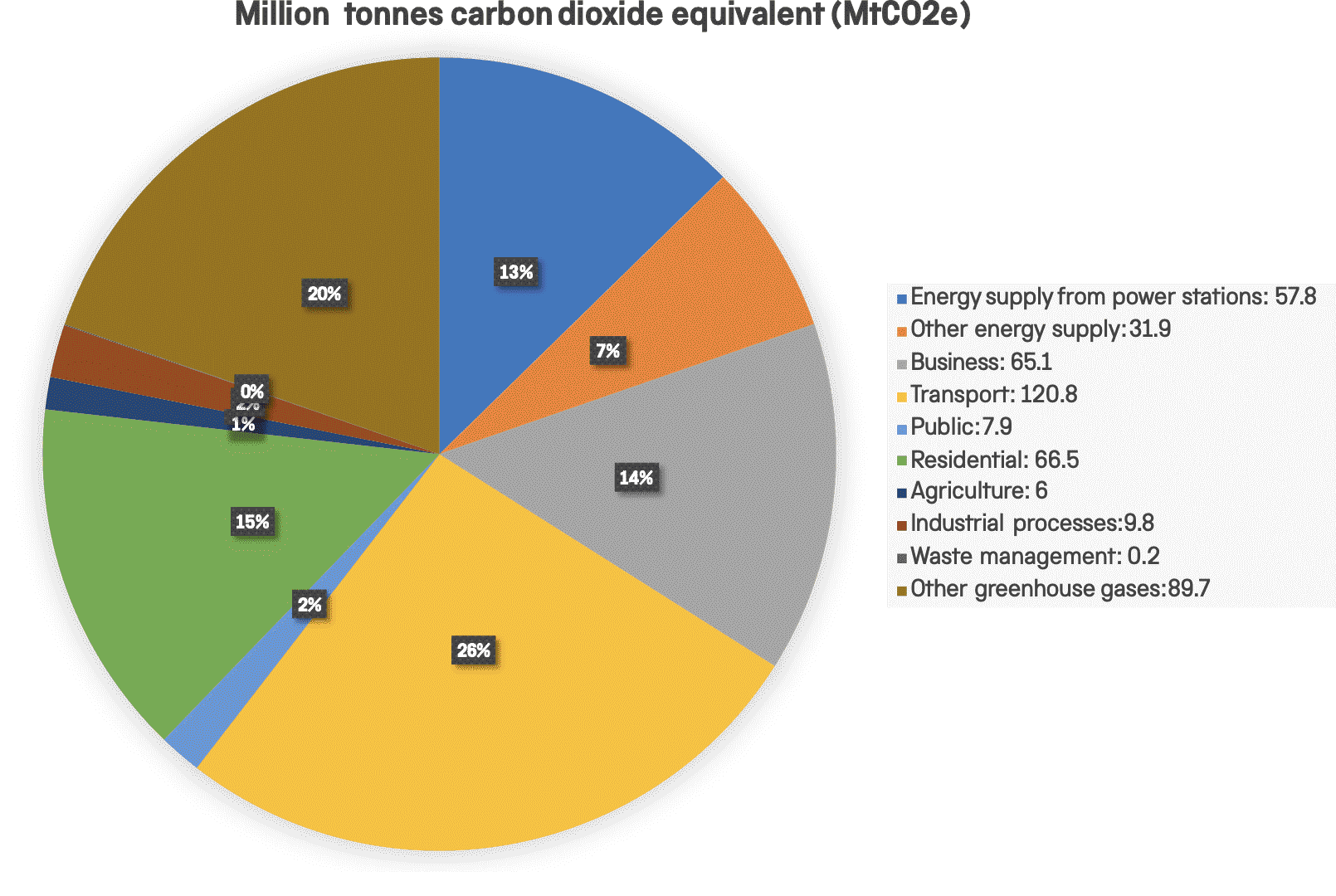
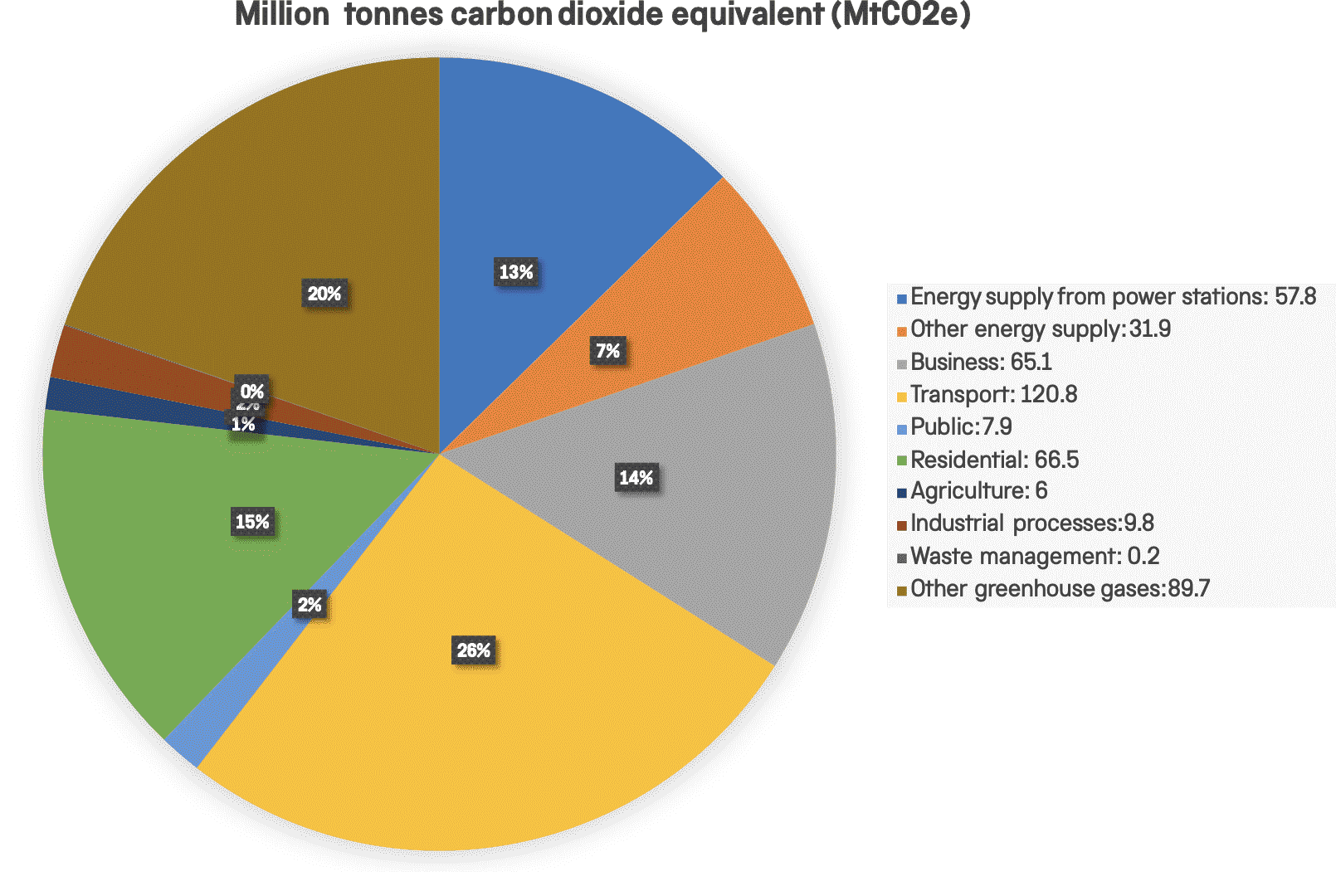
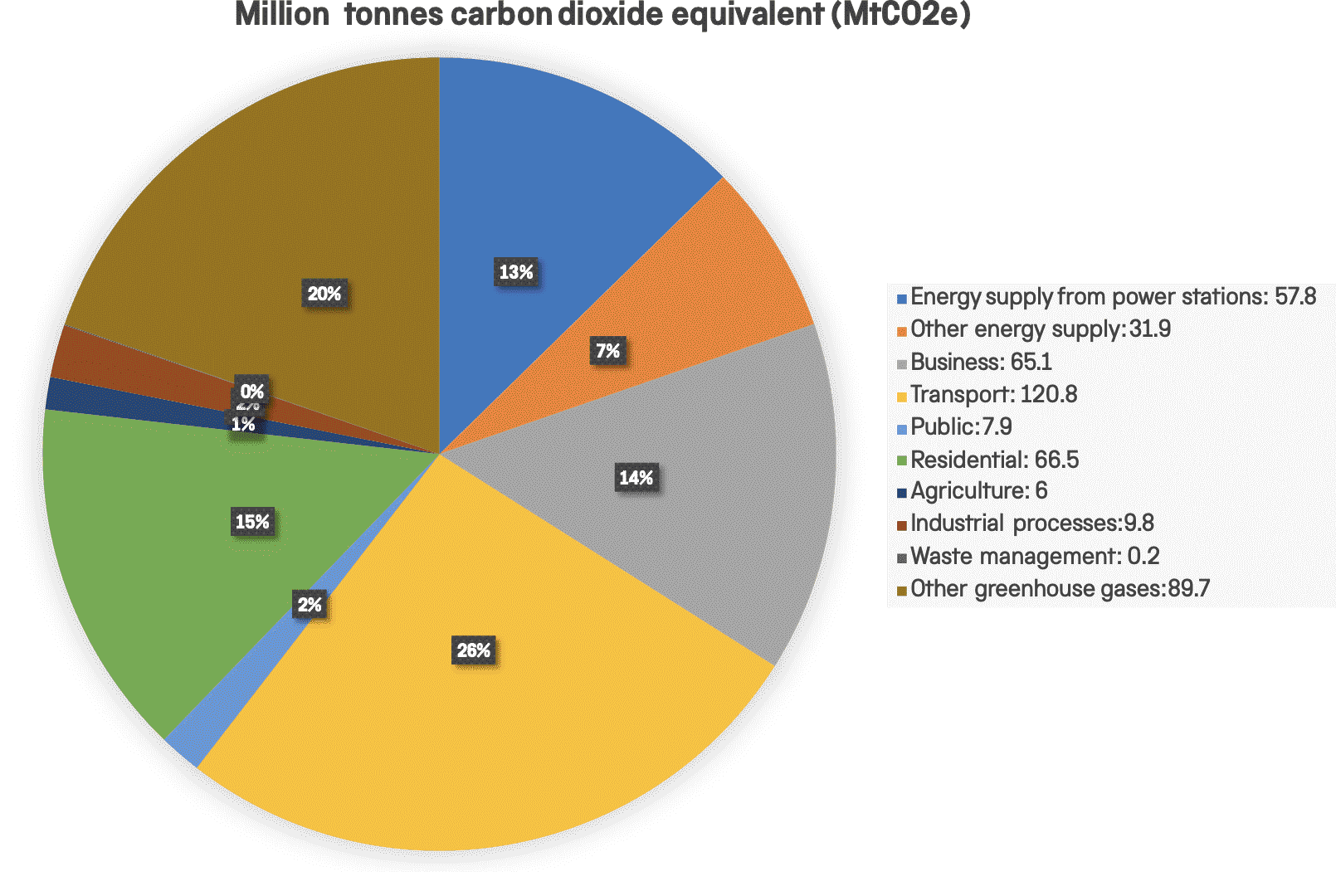
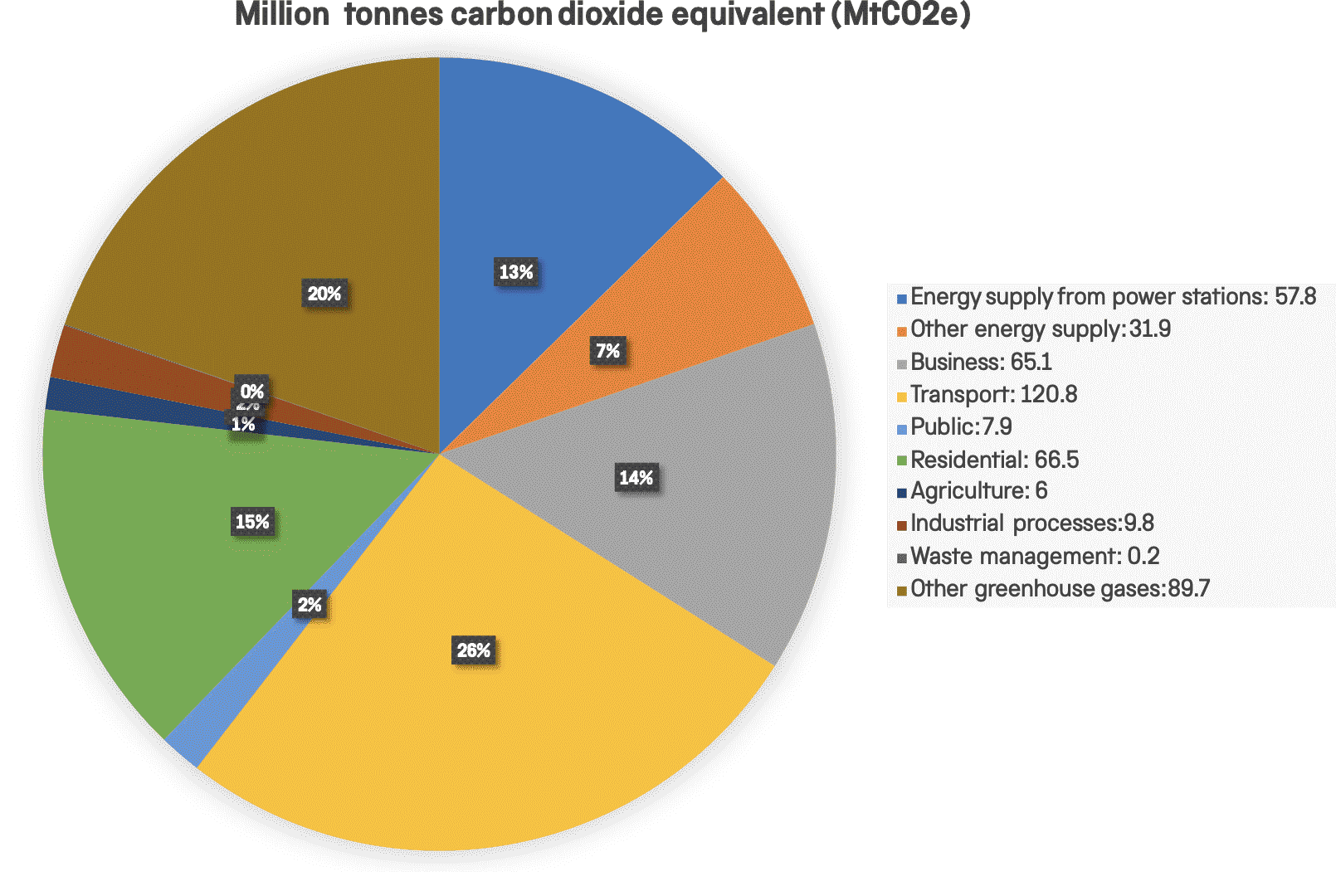
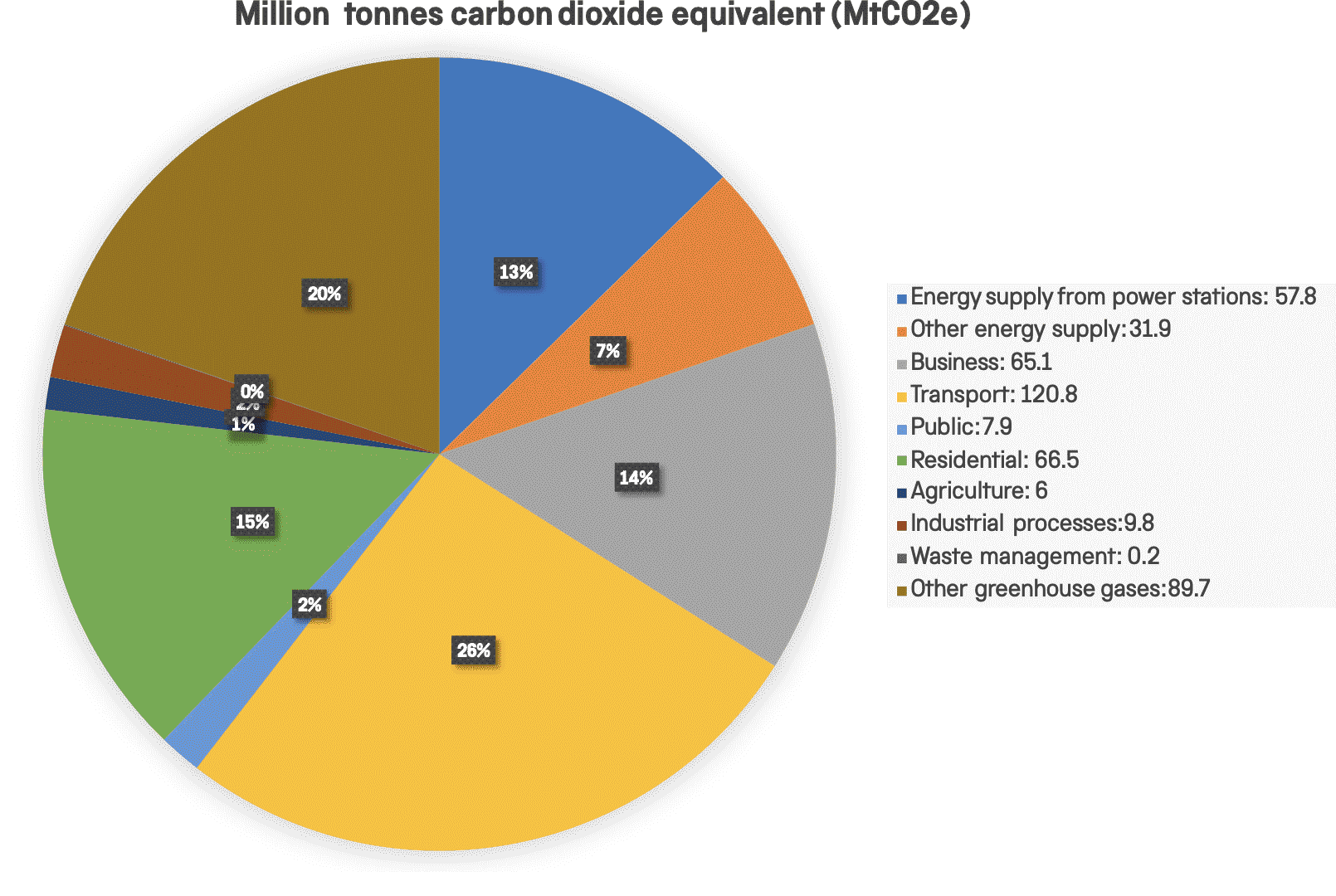
Greenhouse gases are gases in the atmosphere which trap heat and cause the planet to heat up. The NHS creates 5.4% of all UK green house gas emissions. Nitrous oxide, carbon dioxide and fluorinated gases (such as Desflurane) are amongst the worst contributors of greenhouse gases.
Nitrous oxide (laughing gas) is one of the oldest analgesics (pain relief). Synthesised in 1772, it was first used as an analgesic for dentistry in 1844. It is still in common use for childbirth pain relief in the form of Entonox, and as a gas for general anaesthesia. Once released into the atmosphere, it stays there for over 100 years before it breaks down, acting as a potent greenhouse gas and depleting the ozone layer.
Intravenous anaesthesia (total intravenous anaesthesia, or TIVA), where drugs are administered directly into a vein, is a popular method of inducing and maintaining anaesthesia, and is an alternative to using anaesthetic gases. Propofol is one of the most popular intravenous anaesthetic drugs as it often helps reduce postoperative nausea and vomiting. Using TIVA produces more plastic waste, and traces of propofol have been found in waterways; it is toxic to aquatic life in high enough concentrations. Despite this, TIVA has a significantly smaller carbon footprint than using any of the anaesthetic gases.
Carbon dioxide (CO2) is the biggest greenhouse gas in the UK, contributing 81% of total greenhouse gas emissions in 2019. Transport accounts for approximately 1/3 of the CO2 emitted. Healthcare-related journeys make up 13% of the NHS carbon footprint, from patient and staff car travel, to delivering supplies, accounting for 5% of all UK road travel. That is 9.5 billion miles driven annually.

Propofol
intravenous agent, 1991
Propofol (marketed as Diprivan) generally works quickly and patients are awake within a few minutes after the operation with little postoperative sickness or nausea.
The total life cycle of greenhouse gas emissions of propofol infusions are quite small, nearly four orders of magnitude lower than those of desflurane or nitrous oxide.
Forane
inhalation agent,
1982

Drugs
The introduction of intravenous drugs, such as the popular propofol (Diprivan) has been a positive move away from fluorinated inhalation agents, such as halothane, sevoflurane and desflurane, which are powerful greenhouse gases
Total intravenous anaesthesia (TIVA) and Target Controlled Anaesthesia (TCA) for general anaesthesia uses no inhalation agents (gases or vapours). The disadvantages are it creates more medical waste (plastic syringes, tubing, and packaging), and requires electricity for the pump delivery systems. It is easier to overdose and control the depth of anaesthesia with TIVA, but TCA has a computerised system which works out the dose to deliver based on the level of drugs in the blood or brain.
Inhaled anaesthetic agents deplete the ozone layer and act as a greenhouse gas. The biggest contributor to ozone depletion is the agent halothane (commercial name Fluothane). Halothane belongs to the group of chemicals known as hydrofluorocarbons, which are similar to refrigerating agents.
Environmental damage from anaesthetic agents
Total UK nitrous oxide emissions


Agriculture - 70%
Medical use - 1%
Other - 29%


The following video shows how far you would have to drive from London in a petrol car to generate the equivalent carbon emissions as is generated in a typical surgical operation under anaesthesia.
Double-click to edit text
You would have to drive 2273 miles in a petrol car to generate the equivalent carbon emissions as is generated in a typical surgical operation under anaesthesia.
Vaporizers
A vaporizer converts liquid into vapour which can be breathed in. The early pioneers, William Morton, John Snow, and Joseph Clover used vaporizers to deliver ether or chloroform. The flaw with early vaporizers was not being able to control the amount and concentration of vapour being delivered. The addition of gases (a mixture of oxygen and nitrous oxide) as a carrier gas for the anaesthetic vapour changed this as the concentration of the anaesthetic agent was easier to control.
The first anaesthetic machines designed to provide a mixture of gases and anaesthetic vapours were introduced by James Gwathmey and Geoffrey Marshall, but it was Henry Boyle’s ‘Boyles Anaesthetic Machine’ of 1917 that was the most popular and remained in use until the late 1970s.
The introduction of gases improved patient safety through the ability to deliver a known concentration of anaesthetic, but it has had a negative impact on the environment. Vaporizers and the use of gases for anaesthesia are still necessary in many cases, but reducing the use of anaesthetic gases with significant global warming potential, in particular, desflurane and nitrous oxide has the greatest impact on making anaesthesia greener. Making a choice to use oxygen/air as the carrier gas instead of oxygen/nitrous oxide could make a big difference.
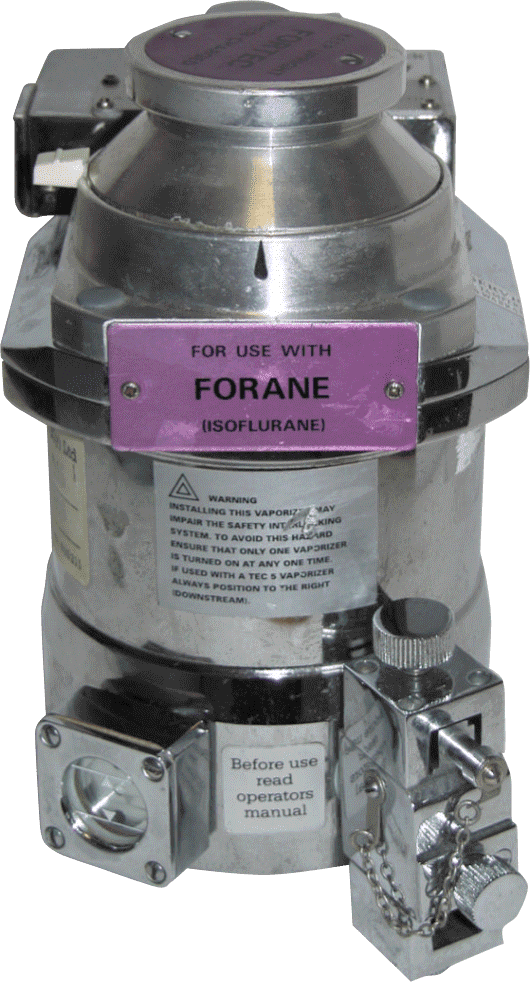
Vaporizer
Vaporizer for use with the fluorinated gas isoflurane, c.1970.
Note the purple colour of the plaque; this matched the colour of the drug packaging to lessen the chance of the wrong drug being used.
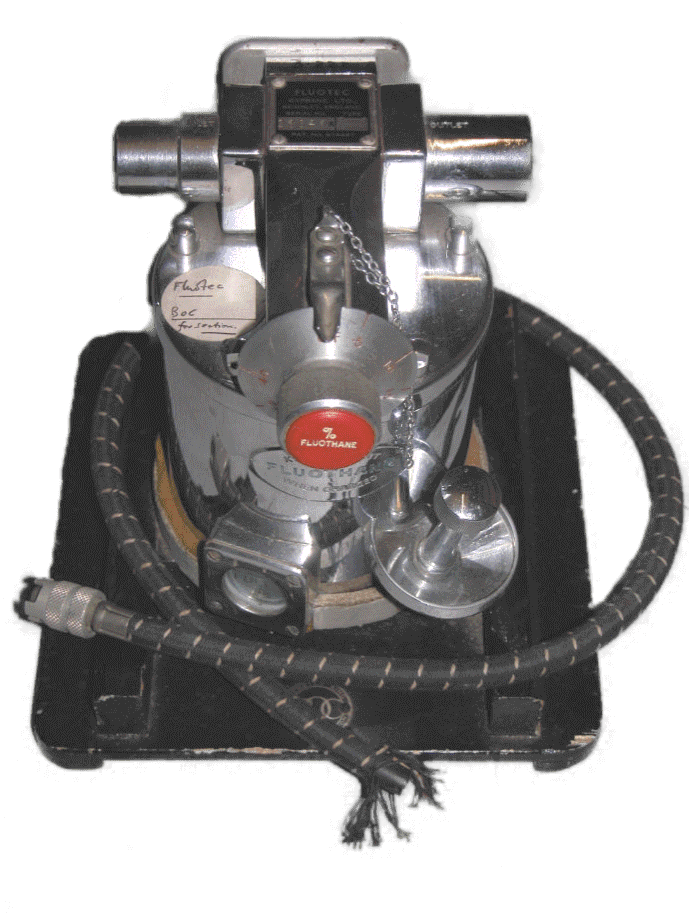
Fluotec vaporizer
This vaporizer was critical in the success of halothane in 1957; it was made for use with halothane only. The Fluotec has a valve to control the amount of carrier gas entering the vapour chamber to vaporise the anaesthetic.
Vaporizer cleaning tools
Cleaning tools for 'Type A' fluotec and Pentec MK.I vaporizers. The kit includes a cleaning rod, Vaseline and an instruction handbook.
Reusable versus single use
Choosing which anaesthetic equipment is reused is based on an assessment of patient safety, infection risk, available facilities and cost. If patient safety can be guaranteed, reusable rather than single use equipment seems an obvious choice, but the environmental impact of the cleaning process for reusables can be high. A balance between single use items and reusable equipment should be achieved.
Reliable equipment is important for patient safety, and the quality of some disposables has been criticised. Plastic laryngoscope blades, used for a procedure called intubation (where a breathing tube is placed in the patient’s airways when they are under anaesthesia), have been blamed for contorting or flexing unexpectedly, which can damage the patient’s larynx. Some also have a poor light source, which can make intubation more difficult.
Environmental life cycle assessments (LCA) are being used to compare the ecological footprint of products and processes. The footprint of reusable medical devices depends on the number of reuses, type of cleaning (low or high level disinfection), sterilisation (steam or chemical) and waste disposal management. One of the concerns with reusable equipment is the small risk that sterilisation does not remove all infective organisms.
There is an LCA comparing the carbon footprint of reusable and single use anaesthetic equipment. Converting from single-use to reusable anaesthetic equipment in the UK, Ireland and Europe would result in an 84% reduction in CO2 emissions. The disadvantage of this is that some disinfectants are highly carbon intensive to produce, and washing reusable equipment uses more water than is used to manufacture single use equipment.

Waste produced after one surgical procedure
Laryngoscopes
A laryngoscope is a tool used for intubation. Originally metal and reusable these are now either completely made of plastic, or have plastic handles and blades. Disposable single use laryngoscopes were introduced over concerns that cleaning did not effectively decontaminate and disinfect the blade, and there was a risk of disease transmission. Some of the plastic blades have been known to flex which can damage the patient’s throat, and the use of plastic and plastic waste has an environmental impact.

Macintosh laryngoscope with a curved blade which lifted the base of the tongue and gave a better view of the vocal cords.
Introduced in 1943 by Professor Robert Macintosh. This design remains the most popular for use in adults; the materials used are now plastic.
Macintosh laryngoscope
Handle
Can contain battery for light source.
Blade
Some versions have a light on the end to guide insertion.
Blade
There is a hinge which allows the blade to fold in for storage
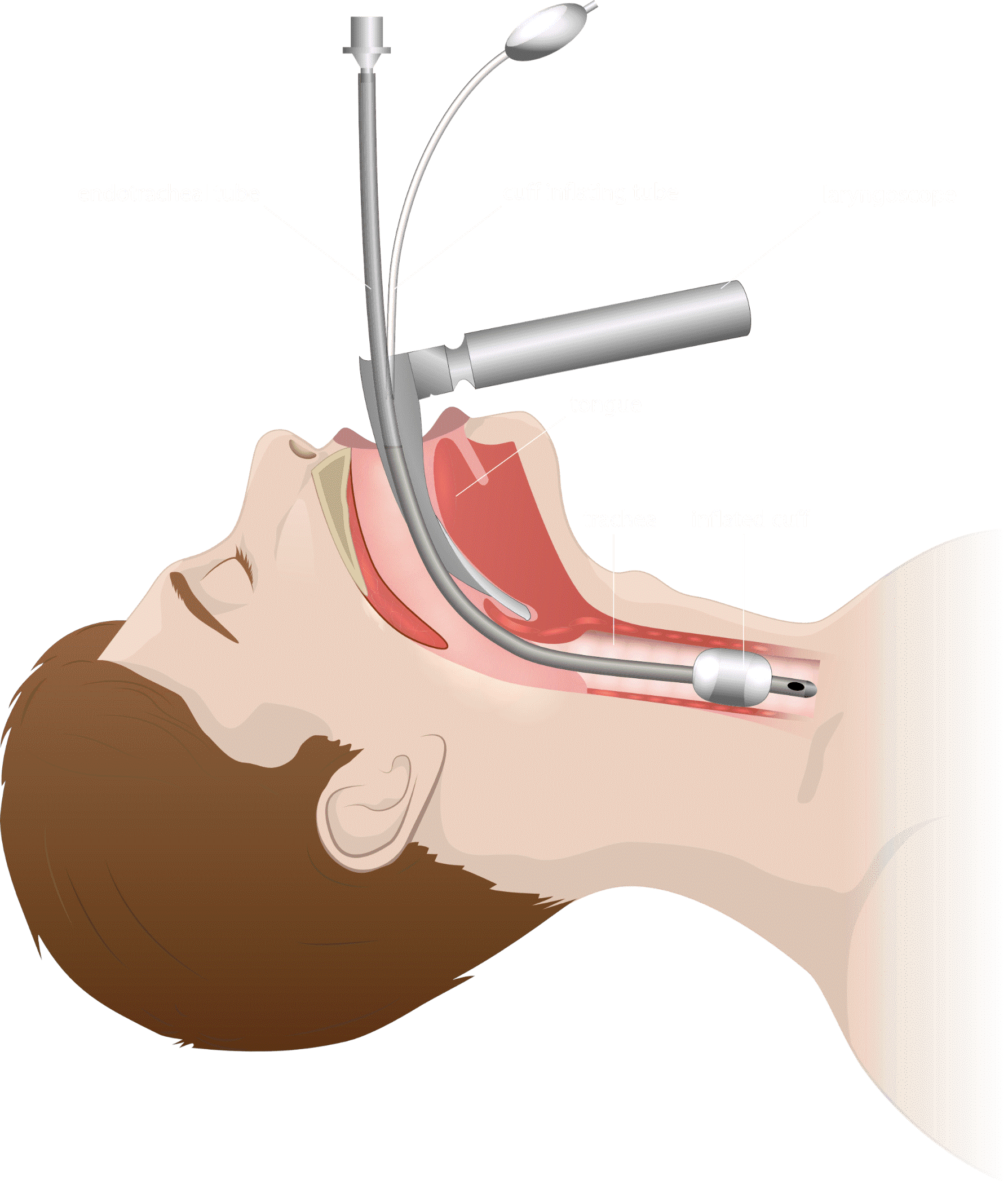
Disposable laryngoscope
Airtraq laryngoscope, dated c.2018.
Disposable laryngoscope blade



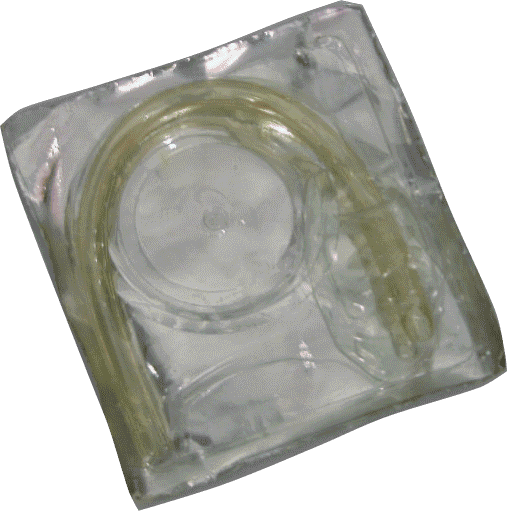
Airways
To maintain a patient’s air passage during anaesthesia, artificial airways are inserted into the mouth and over the tongue. The first artificial metal airway was developed in 1905, followed by many different models. Arthur Guedel introduced his airway in 1933. Unlike its predecessors, the Guedel airway was made of rubber, posing less risk of injury to the patient.
Disposable airways today are made of PVC, while reusable options are made of silicone rubber.


Tubes
Breathing systems are used during anaesthesia to deliver the inhalational (breathable) anaesthetic and oxygen, as well as to remove exhaled carbon dioxide. For this, either masks or tubes are required. Until the introduction of medical PVC in the 1960s, tubes were made of red or black rubber. Black rubber is anti-static, which reduced the risk of explosions or fires during operations using ether or other flammable gases. These tubes were sterilised and reused. Today, there are both disposable as well as reusable options.
Endotracheal tube

Filters
Breathing systems can be reused if they are protected with filters. They protect patients, hospital staff and equipment from contamination by reducing the transmission of microbes in the breathing systems and lowering the infection risk. Filters were first developed in the early 1960s, after the reuse of contaminated breathing bags caused several deaths.
Anaesthetic and respiratory filter, manufactured by Williams, c.1957


Post-tracheostomy
heat and moisture exchange filter.
When a patient is intubated, either during an operation or in intensive care, heat moisture exchangers (HMEs) replicate the natural warming, humidifying and filtering functions of the airway by retaining some of the patient's exhaled heat and moisture.

Connector set
Magill connector set for nasal and oral intubation.
Connector
Portex suction connector
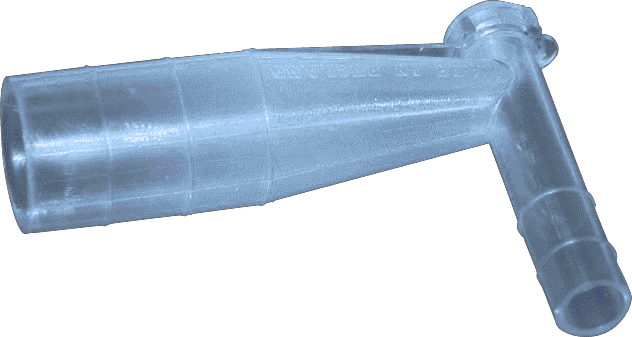
Connectors
Tubes and other components of breathing systems are joined with connectors, which come in different shapes and sizes. Metal connectors were sterilised in an autoclave and reused. Although single-use PVC connectors are widely used today, there are reusable alternatives available.
Medical plastics
Medical plastics were developed slowly and over a period of years, with many different compounds being labelled as ‘plastic’. Key developments came in 1855 and 1907. In 1855, Alexander Parkes invented celluloid (perhaps most famously made into photographic film). Polyvinyl chloride was first polymerised at about the same time (1838-1872). In 1907, Leo Baekeland invented a synthetic hard plastic which he called Bakelite. The wide range of completely synthetic materials that we would recognise today started to be developed around 100 years ago.
Medical plastic is designed to be temperature, chemical and corrosion resistant. Common thermoplastic materials used to produce medical plastic products include polycarbonate, polypropylene and polyethylene. Custom polymers have been formulated for specific medical device uses. Polyvinyl chloride (PVC) and polyethersulfone (PES) have been developed as suitable biocompatible materials. These plastics act and perform without threatening the immune system. This is particularly important for medical equipment that is in direct contact with blood, such as blood transfusion bags and dialysis machines.
The full range of hard and soft plastic is widely used in modern healthcare. Recent attention has focused on packaging and disposable plastics, the potential of biodegradable plastics, and the recycling particularly of hard plastic used in medical equipment.
With greater interest in sustainability, plastics manufacturing is moving from oil-based plastics to recyclable, biodegradable, and even compostable alternatives, many of which are plant-based.
Face Masks
Face mask from anaesthetic apparatus, of unknown type, by British Oxygen Co., 1906-1940
Science Museum Group
© The Board of Trustees of the Science Museum
Anaesthetic gases and vapours are breathed in by a patient through a face mask. Used from the earliest days of anaesthesia, they were originally metal, then rubber was used from the 1930s and plastic from the 1960s. Before the invention of the Clausen Harness in the 1930s, an anaesthetist had to hold the mask over the patient’s face. Dr Clausen’s harness and hook kept the face mask in place without the anaesthetist holding it, which freed them to better observe and monitor the patient.
The new generation of face masks still have these hooks, but they are made from plastic and are often thrown away without being used. Manufacturers are now making face masks available without a hook ring. To further reduce plastic waste, many face masks are now non-PVC and phthalate free.


Clausen harness and ring, c.1930s.
Paediatric facepiece
Plastic facepieces, manufactured by Intersurgical, 2015.
The rubber Clausen harness has three ‘tails’ with holes punched along each one. The holes were hooked over the metal ring which provided a way of tightening or loosening the hold of the facepiece over the patient’s nose and mouth.
The introduction of the rubber facemask helped to provide a softer and better seal to the patient’s face.
The facepiece was sterilised and reused.
Set of four plastic, disposable facepieces with plastic hooks. The hooks are often not used as they make it more difficult and uncomfortable for the anaesthetist to hold the mask and deliver the anaesthetic.


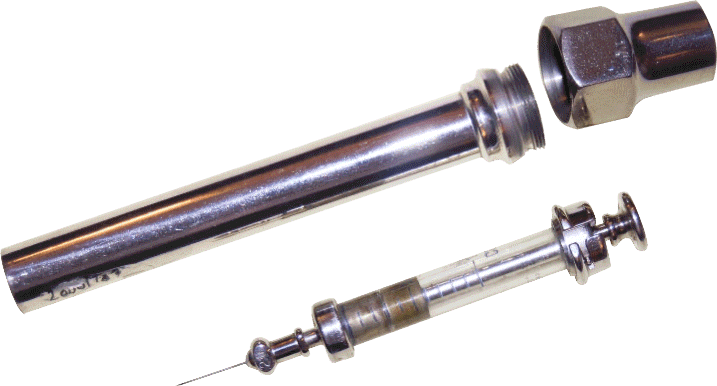
Hypodermic needles and syringes
Hypodermic needles are hollow tubes with sharp tips that contain a small opening. They are used with syringes to inject substances or extract fluids. Syringes predate hypodermic needles by several centuries but could not be successfully used for injections until the development of the hypodermic needle. It was first developed independently by Alexander Wood of Edinburgh and Charles Pravaz of France in 1853. The fine hypodermic needle could be fixed to a syringe, allowing the injection of smaller, precise doses.
Once the danger of infection was understood, needles and syringes were sterilised and reused, until the introduction of medical plastic in the mid-1950s resulted in the advance of disposable syringes and needles

Glass and metal syringe with protective case, manufactured by Weiss.
Plastic disposable syringe marked “USE ONCE ONLY”, c.1950.
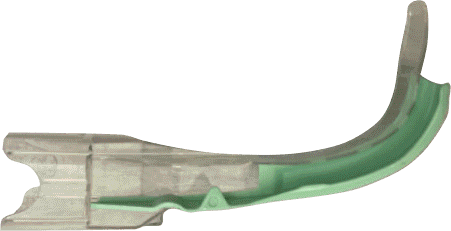
Epidural Anaesthetic
An epidural anaesthetic was first used in clinical surgery in 1921 by Spanish surgeon Fidel Pagés Miravé. A fine tube (an epidural catheter) is threaded through a needle and the end of the tube is positioned in the epidural space in the spine. Local anaesthetic is injected down the tube to provide numbness.
It is now a widely used form of pain relief and can be used as the only anaesthetic for operations such as caesarean section. Intravenous or epidural administration of patient controlled technology in the 1970s meant patients could self administer pain relieving drugs after surgery at the push of a button.
The equipment used for an epidural anaesthetic; the catheter and component parts are plastic and disposable, even the packaging is plastic.
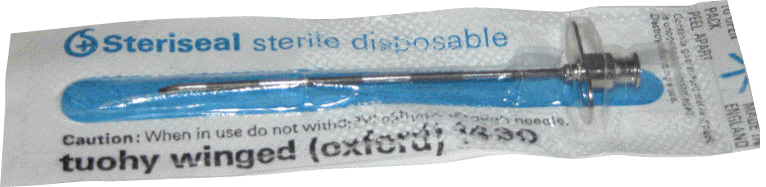

Epidural mini pack
Epidural needle
The impact of the Covid-19 pandemic on the environment
The Covid-19 global pandemic has caused an unprecedented demand on healthcare services across the world. Anaesthetists have found themselves on the front line, caring for those acutely unwell from Covid-19, as well as continuing to deliver elective and emergency surgery and supporting those with non-Covid related illness.
One of the biggest logistical challenges facing the healthcare sector is the supply of personal protective equipment (PPE), needed to minimise the risk of staff contracting Covid-19. The financial, social and environmental cost of providing this PPE has been significant.
In the first six months of the pandemic, the carbon footprint for PPE use in England totalled 106,478 tonnes of CO2. This could be considerably reduced by changing to UK manufacture, rationalising glove use, using reusable rather than disposable PPE, and ensuring as much as possible is recycled.
There have sadly been cases of PPE destined for the NHS being produced under slave labour conditions, highlighting the need to ensure the social costs of healthcare are considered alongside environmental and economic costs.
This global crisis has had a huge impact on how healthcare is delivered, but it has also provided opportunities for change. For example, remote consultations have reduced patient travel.
As we look to a future beyond the pandemic, there is an opportunity to reflect on the positive changes it has brought to healthcare services and the benefits for ourselves and the environment.

Correct!

Incorrect! Try again!


Incorrect! Try again!
Incorrect! Try again!

Quick Quiz
Green house emissions in the NHS is equivalent to the commute of how many NHS staff?
1,300
13,000
130,000
1,300,000
As patients, we can do better too. We can optimise our health before an operation to reduce the need for further hospital and doctor appointments which would require travel. If a patient is considered low risk, they can be offered an online peri-operative assessment. The NHS carries out 3 million operations a year, if online assessments were used for all of those it could save approximately 1 million outpatient appointments, and 6,700 tonnes of carbon emitted through bus or car journeys.
A greater look at disease prevention is also essential to avoid the need for operations and drugs. Social prescribing, which links people to community support to improve their health and wellbeing, is another way of reducing the pressure on healthcare services.
The NHS is committed to improvement. Their green ambitions are outlined in the 2020 Delivering a Net Zero NHS, with a pledge to being carbon neutral by 2045.
Raising awareness and making changes, whether big or small, are making a difference, but there is a long way to go to reach the goal of net-zero carbon emissions, and not much time to accomplish it. Understanding the impact of anaesthesia on the environment means those changes can be made within the specialty as efficiently as possible.
Making different choices around anaesthetic agents, for example choosing not to use an anaesthetic gas, is one way the specialty can lessen their carbon footprint. Technology is being developed that captures volatile anaesthetic gases from the atmosphere in the operating theatre, purifies and recycles it for reuse. Nitrous oxide capture is widely used in Sweden and is currently being trialled in a number of hospitals in the UK.
Newcastle upon Tyne Hospitals NHS Foundation Trust were the first healthcare organisation in the world to declare a climate emergency. They aim to become carbon neutral by 2040. Changes made include renewable energy to power the hospitals, zero waste to landfill, electric patient buses, reusable sharps boxes and recycling over 40% of non-clinical waste. The environment is becoming part of students’ education, with Newcastle University Medical School teaching students sustainable practice.
How we can do better
Acknowledgements
The Anaesthesia Heritage Centre would like to thank the exhibition co-curator Dr Chris Allen (Environmentally Sustainable Anaesthesia Fellow 2020-21) and Heritage Volunteers for their expertise, guidance and support.
Events
We are running a number of events linked to the exhibition across the year, from family workshops to talks. These are bookable via our events page or EventBrite.
Further reading
If you would like to find out more about the history of anaesthesia and the work of the Anaesthesia Heritage Centre, please check out our website, or follow us on Twitter or Facebook.
Give us your feedback
